📊 OCD in the UK – Facts, Prevalence, and Treatment Access
OCD in the UK: Over the years, obsessive-compulsive disorder (OCD) has gained recognition as a significant mental health condition affecting many in the UK. With an estimated 1.2% of the population experiencing OCD, understanding its symptoms and prevalence is vital for you to identify and seek help. Access to treatment options varies, with many facing challenges in getting the support they need. This blog post will provide you with important facts, insights into prevalence, and the available treatment paths so you can make informed decisions about your mental health.
Key Takeaways:
- Obsessive-Compulsive Disorder (OCD) affects approximately 1.2% of the UK population, indicating a significant mental health concern.
- OCD can manifest in various forms, with common obsessions including fears of contamination, harm, and intrusive thoughts.
- Access to effective treatments, such as cognitive behavioural therapy (CBT) and medication, remains inconsistent across different regions in the UK.
- Public awareness and understanding of OCD are growing, yet many individuals still face stigma, hindering their willingness to seek help.
- Early diagnosis and intervention are vital for improving outcomes, emphasising the need for better education and resources for both healthcare professionals and the public.
The Alarming Statistics: OCD Prevalence in the UK
Approximately 1.2% of the UK population is estimated to experience obsessive-compulsive disorder in any given year. This figure might seem minor, but it translates to over 800,000 individuals grappling with intrusive thoughts and compulsive behaviours that can severely impact day-to-day functioning and quality of life. Understanding these numbers highlights the need for greater attention and resources towards effective treatment and support.
National Surveys and Data Findings
Recent national surveys, including the Adult Psychiatric Morbidity Survey, reveal that OCD often emerges in late adolescence or early adulthood, with an average onset age between 18 and 24 years. The data indicates that many affected individuals hesitate to seek assistance, leading to a significant portion remaining undiagnosed and untreated for years. This contributes to the long-term effects on mental health and overall well-being.
Demographic Variations in OCD Cases
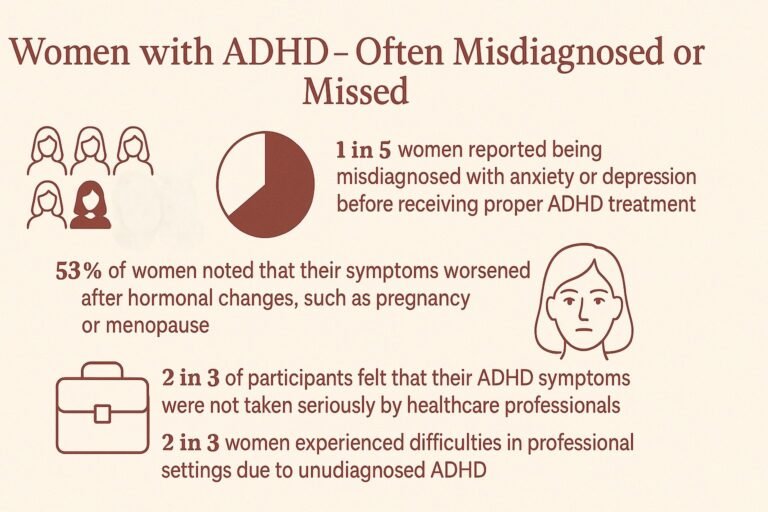
Demographic factors play a substantial role in the prevalence of OCD, with variations observed across age, gender, and socioeconomic status. Research shows that women are slightly more likely to develop OCD than men, although the severity of symptoms can vary significantly between the sexes. Additionally, rates of diagnosis seem higher among individuals from urban areas compared to rural settings, potentially due to increased awareness and access to mental health resources.
When examining the implications of these demographic variations, you’ll find that cultural attitudes towards mental health may influence both reporting rates and help-seeking behaviours. For instance, young adults are often more open to discussing their struggles, increasing visibility for OCD among this cohort. Conversely, older generations may experience a stigma surrounding mental health, leading to underreporting and a lack of access to vital treatments. This understanding signals to you the importance of tailoring support and outreach efforts to particular demographic groups to ensure everyone receives the care they need.
The Emotional Toll: Understanding the Impact of OCD
Obsessive-compulsive disorder can profoundly affect your emotional wellbeing, leading to persistent feelings of anxiety, fear, and distress. The relentless cycle of obsessions and compulsions creates a sense of being trapped, often resulting in shame or frustration about the inability to control one’s thoughts and behaviours. Many individuals report feeling isolated, as if they are the only ones experiencing these challenges, which can exacerbate feelings of loneliness and depression.
Daily Life Disruptions for Sufferers
Your daily life can be significantly disrupted by OCD, as routines may revolve around compulsive behaviours that consume hours of your day. You might find it difficult to focus on work or maintain social relationships due to the intrusive thoughts that demand immediate attention. Even simple tasks like getting dressed or leaving the house can become monumental challenges, impacting your overall quality of life.
The Stigmatisation of Mental Health Disorders
The societal stigma surrounding mental health disorders, including OCD, can heighten your feelings of embarrassment and isolation. Often, you may feel pressured to conceal your struggles from others, fearing judgement or misunderstanding. This stigma not only makes it harder to seek help but also contributes to the perception that mental health issues are less valid than physical ailments.
Stigmatisation manifests in various ways, from terminology that trivialises mental health conditions to the lack of awareness about OCD’s complexities. You may encounter individuals scoffing at compulsions as mere quirks or misconceptions surrounding the disorder itself, which can perpetuate the feeling that your experiences are invalid. Education and advocacy are critical; studies show that increased awareness can significantly reduce stigma and encourage individuals to seek help, fostering a more supportive environment in which you can thrive and openly discuss your challenges.
Pathways to Diagnosis: How OCD is Identified
Identifying Obsessive-Compulsive Disorder (OCD) involves a structured approach, often beginning with a detailed assessment by a healthcare professional. You may be asked about your symptoms, thoughts, and behaviours, alongside their duration and severity. Standardised questionnaires and interviews play a pivotal role in accurately diagnosing OCD, ensuring no other mental health conditions are contributing to your difficulties.
Criteria for OCD Diagnosis
According to the DSM-5 and ICD-11, the diagnosis of OCD is based on the presence of obsessions and/or compulsions that are time-consuming (more than one hour per day) and cause significant distress or impairment in functioning. Obsessions are unwanted, intrusive thoughts, while compulsions are repetitive behaviours performed in response to the obsessions or according to rigid rules.
The Role of Mental Health Professionals
Mental health professionals, such as psychologists and psychiatrists, play an important role in diagnosing and treating OCD. They utilise a combination of clinical interviews, behavioural assessments, and standardised tests to determine the nature and extent of your condition. Their expertise ensures accurate diagnoses and personalised treatment plans, often incorporating cognitive-behavioural therapy (CBT) and medication when necessary.
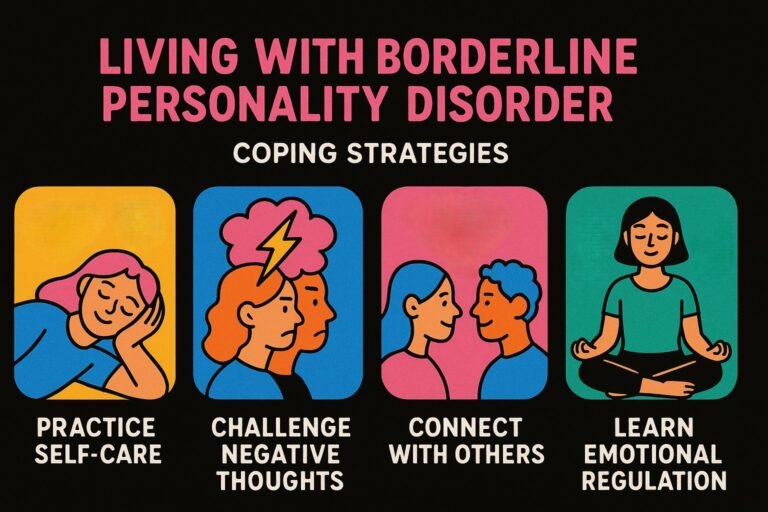
Engaging with a mental health professional can significantly impact your journey toward managing OCD. These specialists are trained to understand the nuances of anxiety disorders, including OCD’s complex interplay of obsessive thoughts and compulsive behaviours. Through tailored therapeutic interventions, they provide you with coping strategies, support, and education about your condition, enabling you to better navigate the challenges you face daily. This tailored approach empowers you to find effective relief and step towards improved mental health.

Bridging the Gap: Accessing Treatment in the UK
Obtaining effective treatment for OCD in the UK can often feel like navigating a complex maze. Although many therapeutic options are available, understanding how to access these resources is paramount for individuals seeking relief. Your journey may involve multiple routes, including NHS services, private practices, or community initiatives, each offering varying levels of care and success. The key lies in knowing where to turn and how to advocate for yourself when faced with delays or barriers.
Availability of Therapeutic Options
In the UK, a range of therapeutic options for OCD are accessible, including Cognitive Behavioural Therapy (CBT), Exposure and Response Prevention (ERP), and medication like SSRIs. These treatments are supported by the National Institute for Health and Care Excellence (NICE) guidelines, providing a framework for quality care. Many individuals find success through a combination of therapy and medication, tailoring their approach to suit personal needs and preferences.
Challenges in Treatment Accessibility
Despite the array of treatment options, accessing them poses significant challenges for many individuals. Long waiting lists within NHS mental health services can be discouraging and often lead to reduced motivation and worsening symptoms. Limited availability of qualified therapists, especially in rural areas, compounds the issue, making it harder for you to gain timely support. Understanding these challenges can empower you to seek alternative routes or advocate for better access to care.
Long waiting times for therapy can extend beyond six months in some regions, as reported by NHS data, effectively stalling your journey towards recovery. The disparity in service availability, especially in less urban areas, exacerbates feelings of isolation and frustration when pursuing treatment. Additionally, financial constraints may restrict access to private therapy, leaving some without appropriate interventions. Support groups and online resources can bridge these gaps, but the reality remains that many still struggle to find consistent and effective assistance.
Innovative Approaches: The Future of OCD Management
Advancements in the management of OCD are rapidly evolving, offering fresh optimism for those affected. Innovative therapies, including digital mental health solutions and neurostimulation techniques, hold promise in enhancing traditional treatment methods. These emerging strategies not only aim to improve therapeutic outcomes but also to minimise the burden of symptoms on daily life. As research progresses, these advancements may redefine how you experience and cope with OCD.
Emerging Therapies and Technologies
New therapies and technologies are reshaping OCD treatment landscapes. For instance, virtual reality therapy is gaining traction, allowing you to confront fears in a controlled virtual environment, which can desensitise anxiety triggers. Additionally, digital self-help apps provide practical coping strategies and real-time assessments, making it easier to track progress and tailor treatment to your specific needs.
The Importance of Public Awareness and Education
Heightened awareness and education around OCD can significantly impact the lived experience of those affected. By fostering understanding in the community, you contribute to reduction in stigma and misinformation, paving the way for more people to seek help. Campaigns and workshops can provide insights into OCD symptoms, treatments, and coping strategies, creating a supportive environment tailored to individual needs.
Engaging the public in conversations about OCD can facilitate more informed discussions about mental health. Schools, workplaces, and local communities can benefit from workshops that educate individuals about OCD, its prevalence, and the available treatments. This proactive stance allows you to not only advocate for yourself but also support others who may be silently struggling. Awareness reduces stigma, encouraging those affected to seek the help they deserve while promoting a culture of empathy and understanding across society.
To wrap up
Taking this into account, it’s crucial for you to understand the prevalence of OCD in the UK and the challenges surrounding treatment access. With 1 in 100 adults experiencing OCD, awareness and early intervention are vital. Your journey towards management may be supported through various therapeutic options, but accessibility can pose challenges. By recognising the importance of seeking help and advocating for better services, you can take proactive steps towards improving your mental health and understanding of OCD.
FAQ
Q: What is OCD and how does it manifest in individuals?
A: Obsessive-Compulsive Disorder (OCD) is a mental health condition characterised by persistent, unwanted thoughts (obsessions) and repetitive behaviours or mental acts (compulsions) that an individual feels driven to perform. Individuals with OCD may experience intense anxiety due to their obsessions and engage in compulsions to try to alleviate that anxiety. Common themes include fears of contamination, harm, or a need for orderliness.
Q: What is the prevalence of OCD in the UK?
A: Research indicates that approximately 1.2% of the population in the UK will experience OCD at some point in their lives. It can affect people of all ages, including children, but often begins in adolescence or early adulthood. Despite its prevalence, OCD is frequently misunderstood, which may contribute to delays in diagnosis and treatment.
Q: What treatments are available for OCD in the UK?
A: Effective treatments for OCD usually include Cognitive Behavioural Therapy (CBT), particularly a specific form called Exposure and Response Prevention (ERP). In certain cases, medication such as selective serotonin reuptake inhibitors (SSRIs) may be prescribed. Access to treatment can vary, with many individuals being referred through their GP or accessing private services for quicker support.
Q: Are there adequate resources and support for those suffering from OCD in the UK?
A: Yes, there are numerous resources available for individuals dealing with OCD in the UK. Organisations such as OCD Action and the National OCD Foundation provide support, information, and access to online forums. Additionally, many NHS services offer psychological therapies, though waiting times can vary. It is advisable for individuals to reach out to mental health professionals for guidance tailored to their needs.
Q: How can family and friends support someone with OCD?
A: Supporting someone with OCD involves being patient and understanding their challenges without judgment. It is important to listen and provide emotional support, while also encouraging them to seek professional help. Educating oneself about OCD can also be beneficial, as it fosters a supportive environment. Additionally, helping them engage in enjoyable activities can provide relief from their symptoms.
Check your mental health symptoms on the NHS.
Mental Health in the UK | Mental Health Conditions | Access to Support and Services