📊 Eating Disorders in the UK – Who Is Affected and How
With 1.6 million individuals in the UK affected by eating disorders, it’s necessary to understand who these people are and the impact on their lives. This post will help you identify the different types of eating disorders, their symptoms, and the demographics most commonly affected.
You’ll discover how societal pressures and mental health challenges intertwine with these disorders, shedding light on the importance of recognition and support. Understanding these aspects can empower you to make informed decisions, whether for yourself or someone you care about.
Key Takeaways:
Recognising the scope and impact of eating disorders in the UK is crucial for effective support and treatment.
- Eating disorders affect individuals across all age groups, with the highest prevalence observed among teenagers and young adults.
- Both genders are impacted, although there is a higher incidence of eating disorders among women compared to men.
- Risk factors include genetic predisposition, psychological issues, societal pressures, and traumatic experiences.
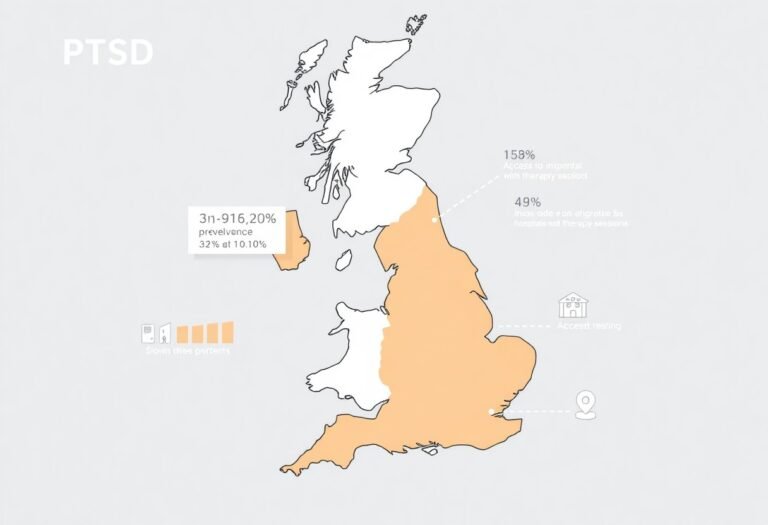
- Access to treatment and support varies significantly, with many individuals facing long waiting times for specialist care.
- Early intervention and awareness are vital in reducing the severity and duration of eating disorders.
Unmasking the Demographics: Who Is Most Impacted?
Statistics reveal that around 1.25 million people in the UK are affected by an eating disorder. A significant number of these individuals remain undiagnosed. This issue predominantly impacts young adults and teenagers. Females are disproportionately affected, comprising about 90% of cases. Increasing numbers of males are also seeking help, challenging old stereotypes associated with these disorders.
Age and Gender Disparities in Eating Disorders
Research highlights distinct age and gender disparities when it comes to eating disorders. Typically, females develop conditions like anorexia and bulimia in their late teens and early twenties.
Men tend to experience such challenges slightly later, often in their twenties or thirties. The societal pressures faced during adolescence can exacerbate these disorders.
Socioeconomic Influences on Anorexia, Bulimia, and Binge Eating
Socioeconomic status plays a pivotal role in the prevalence of eating disorders. Those from lower-income backgrounds face heightened risk for conditions such as anorexia, bulimia, and binge eating.
Limited access to mental health resources and societal pressures exacerbate these issues.
In households where financial stress is common, the urgency to conform to unrealistic body ideals can lead to unhealthy eating behaviours.
Access to adequate healthcare can drastically vary based on socioeconomic status. Individuals in lower income brackets often encounter barriers to treatment, including financial constraints and a lack of local services. This situation can create a cycle where untreated eating disorders further entrench economic difficulties.
Furthermore, those in lower socio-economic areas may be exposed to higher levels of stress and unhealthy living conditions. This can push them toward binge eating as a coping mechanism.
Addressing these socioeconomic influences is important for effective intervention and support for those affected.

The Cultural Constructs: Media Influence and Body Image
The pervasive influence of media on societal perceptions of body image cannot be underestimated. Advertising campaigns, television shows, and films promote idealised body types that skew public perception of what is considered normal or healthy.
This distortion fuels unrealistic expectations and leads individuals to punish themselves physically and emotionally in pursuit of an unattainable appearance.
The effects of such pressure can be devastating, particularly among the young, who are highly susceptible to social comparison and internalising these harmful standards.
The Role of Social Media in Shaping Perceptions
Social media platforms are amplifying the issues surrounding body image. They create a distorted reality where curated perfection appears typical. Influencers showcase edited photos that set unattainable standards for their followers.
This constant exposure fosters a culture of comparison, making you feel inadequate or pressured to change your appearance. Studies indicate that time spent on social media correlates with increased dissatisfaction regarding one’s own body, particularly among teenagers and young adults.
How Traditional Media Reinforces Unrealistic Standards
The traditional media landscape is filled with representations that reinforce unrealistic beauty standards, predominantly highlighting slim figures and flawless skin. Films, magazines, and advertisements often feature a narrow spectrum of beauty, typically promoting a size zero to four as the norm. Such portrayals convey the subtle message that appearance equates to worth, compelling individuals to chase these superficial ideals.
The result is an insidious cycle of discontent and pursuit of unrealistic body shapes, contributing to the alarming rise in eating disorders.
For example, a study by the National Eating Disorders Association found that exposure to media idealising thinness increases the risk of developing eating disorders. The portrayal of women in advertisements, often heavily edited and airbrushed, creates a mental image that is notably skewed from reality.
Men are not exempt from this influence either; with rising trends in depicting hyper-masculinity and low body fat percentages in male models, men often feel undue pressure to conform to these stringent ideals.
Symptoms and Warning Signs: Recognising the Red Flags
Awareness of the symptoms associated with eating disorders can empower you to identify potential issues early. Key warning signs include significant weight loss or gain, obsession with calorie counting, and changes in eating habits or routines.
Emotional symptoms may manifest as increased anxiety, mood swings, or withdrawal from social activities, prompting a deeper examination of an individual’s relationship with food and body image.
Physical and Emotional Indicators of Eating Disorders
Physical indicators often encompass drastic weight fluctuations, brittle hair and nails, or gastrointestinal issues. You might also notice fluctuations in energy levels or a constant feeling of fatigue.
Emotionally, you may observe behaviours such as isolation, perpetuating negative self-talk, or an unusual preoccupation with food or exercise. These signs are all signals that should not be overlooked.
How to Approach a Loved One Showing Symptoms
Approaching a loved one who exhibits symptoms of an eating disorder requires a delicate balance of compassion and honesty. Start by choosing a private and safe environment where they feel comfortable discussing personal matters.
Express specific observations without placing blame, and highlight your concern for their well-being. Maintaining an open dialogue will encourage them to share their feelings and may lead them to seek professional help.
When engaging with someone showing symptoms, focus on your genuine concern for their health rather than making assumptions about their behaviour. You could say, “I’ve noticed you seem really stressed about food lately, and I’m worried about you.”
Encouraging a non-judgmental conversation fosters trust and allows them to open up about their struggles. Offering to accompany them to a healthcare professional can also provide significantly needed support, reiterating that seeking help is a positive step.
Navigating Treatment Options: Pathways to Recovery
Exploring treatment options for eating disorders involves a multifaceted approach tailored to your specific needs. Combining therapy, medical intervention, and support from loved ones significantly enhances your chances of recovery.
Effective treatments often encompass cognitive-behavioural therapy (CBT), nutritional counselling, and medical supervision, ensuring that every aspect of the disorder is addressed.
Your support network can significantly influence your recovery, providing imperative emotional and practical assistance. Family and friends may offer encouragement or accompany you to treatment sessions, fostering an environment of understanding and positivity.
Support groups, whether in-person or online, enable connections with others who understand your struggles, instilling a sense of community and shared experience.
Professional intervention typically begins with a thorough assessment by a healthcare provider, leading to personalised treatment plans. Therapy, such as CBT or dialectical behaviour therapy (DBT), plays a vital role in addressing the psychological aspects of eating disorders. In some cases, medication prescribed by a psychiatrist may also be beneficial to manage co-occurring mental health issues. Regular follow-ups with medical professionals help monitor your health and progress, ensuring a comprehensive approach to recovery.
Role of Support Networks in the Recovery Journey
Your support network can significantly influence your recovery, providing imperative emotional and practical assistance. Family and friends may offer encouragement or accompany you to treatment sessions, fostering an environment of understanding and positivity. Support groups, whether in-person or online, enable connections with others who understand your struggles, instilling a sense of community and shared experience. This network can empower you to confront challenges and celebrate milestones along the way.
Building a strong support network can be one of the most transformative elements of your recovery journey. Engaging with family members, friends, or support groups allows you to share experiences and receive shared insights. Many find strength in connecting with others who have faced similar battles, reducing feelings of isolation.
The encouragement and understanding from your support system can be pivotal in navigating tough moments and reinforcing your commitment to recovery. They can also help hold you accountable, reminding you of your goals and progress as you work towards a healthier, happier life.
The COVID-19 pandemic has acted as a catalyst, exacerbating the prevalence of eating disorders across the UK. Reports indicate that more individuals have sought help for conditions like anorexia and bulimia, with helplines experiencing a significant surge in calls. This escalating demand for support illustrates the profound relationship between societal disruptions and mental health issues, underscoring the need for immediate intervention.
The COVID-19 pandemic has undeniably acted as a catalyst, exacerbating the prevalence of eating disorders across the UK. Reports indicate that more individuals have sought help for conditions like anorexia and bulimia, with helplines experiencing a significant surge in calls.
This escalating demand for support illustrates the profound relationship between societal disruptions and mental health issues, underscoring the need for immediate intervention.
Increased Stressors During the Pandemic
During the pandemic, you faced numerous stressors that amplified anxiety and uncertainty. Isolation, fear of illness, and economic worries contributed to heightened emotional distress. The lockdowns disrupted daily routines, diminishing access to a supportive community and increasing reliance on unhealthy coping mechanisms.
Long-term Effects on Mental Health and Eating Behaviours
The long-term effects of the pandemic on mental health and eating behaviours are becoming increasingly evident. You may find that the stressors experienced during this time have caused lingering anxiety, potentially exacerbating or triggering eating disorders. Research shows that many individuals have reported a shift in their relationship with food, often resulting in disordered patterns that can persist even after life returns to normal.
For those grappling with the aftermath of the pandemic, the intertwined nature of mental health and eating behaviours creates a complex web of challenges. Common experiences include feelings of shame, guilt, and an overwhelming preoccupation with food and body image. Many people reported increased binge-eating episodes or restrictive habits as a means of exerting control amidst chaos.
As you navigate the long-term repercussions of these experiences, understanding the lasting impact on your mental health is vital. This knowledge is crucial in seeking appropriate support and establishing healthier coping strategies.
To wrap up
In conclusion, understanding the landscape of eating disorders in the UK is imperative for recognising their impact on you and those around you. These disorders do not discriminate, affecting individuals across various demographics, including age, gender, and socioeconomic background.
Being informed about the signs and symptoms enables you to identify when support is needed, whether for yourself or someone you care about.
FAQ
Q: What are the most common types of eating disorders affecting people in the UK?
A: The most prevalent eating disorders in the UK include anorexia nervosa, bulimia nervosa, and binge eating disorder. Anorexia is characterised by extreme weight loss and a fear of gaining weight, while bulimia involves cycles of binge eating followed by purging. Binge eating disorder, on the other hand, consists of episodes of eating large quantities of food without purging. Other less common disorders include avoidant/restrictive food intake disorder (ARFID) and pica, which involves craving and consuming non-food substances.
Q: Who is most at risk of developing an eating disorder in the UK?
A: Eating disorders can affect individuals of all ages, genders, and backgrounds. However, they are particularly prevalent among young people, especially females aged between 13 and 25. Socio-cultural factors, such as societal pressure to conform to certain body standards, can contribute to the risk. Additionally, individuals with a family history of eating disorders, mental health issues, or those experiencing significant life changes or stress may also be more susceptible.
Q: What are the psychological factors associated with eating disorders?
A: Psychological factors play a significant role in the development of eating disorders. Individuals may face issues such as low self-esteem, perfectionism, anxiety, and depression. These emotional struggles can lead to unhealthy coping mechanisms, with food and body image becoming central to their identity. Therapy and psychological support are often crucial components of recovery, as addressing these underlying emotional issues can facilitate healthier behaviours and attitudes toward food.
Q: How are eating disorders treated in the UK?
A: Treatment for eating disorders typically involves a combination of psychological therapy, nutritional education, and medical support. The most common therapies include Cognitive Behavioural Therapy (CBT), which aims to change negative thought patterns, and family-based therapy, particularly for adolescents. Nutritional counselling helps individuals develop a healthier relationship with food. In severe cases, inpatient or residential care may be necessary to provide intensive support and monitoring.
Q: What resources are available for individuals struggling with eating disorders in the UK?
A: The UK offers various resources for those dealing with eating disorders. Organisations such as BEAT (Beat Eating Disorders) provide help via a helpline, online support groups, and information about local services. The NHS also has dedicated services for mental health support, including specialised services for eating disorders. Additionally, many charities and private clinics offer therapy and support tailored to individuals experiencing these conditions.
Check your mental health symptoms on the NHS.
Mental Health Conditions | Mental Health in the UK | What Is Mental Health?