📊 Schizophrenia in the UK – Prevalence, Access, and Misconceptions
Most people are unaware that approximately 1 in 100 individuals in the UK are affected by schizophrenia, a serious mental health condition that can lead to significant challenges in daily life. Understanding your access to effective treatment options is necessary, as many still face barriers due to stigma and misinformation. By dispelling common misconceptions, you can gain a clearer insight into the realities of living with this condition, enhancing your awareness and empathy towards those impacted by it.
Key Takeaways:
- Schizophrenia affects approximately 1% of the UK population.
- Access to mental health services remains inconsistent across different regions.
- There is a significant stigma associated with schizophrenia, leading to misunderstandings.
- Early intervention can improve outcomes for individuals diagnosed with the condition.
- Education and awareness initiatives are necessary to combat misconceptions surrounding schizophrenia.
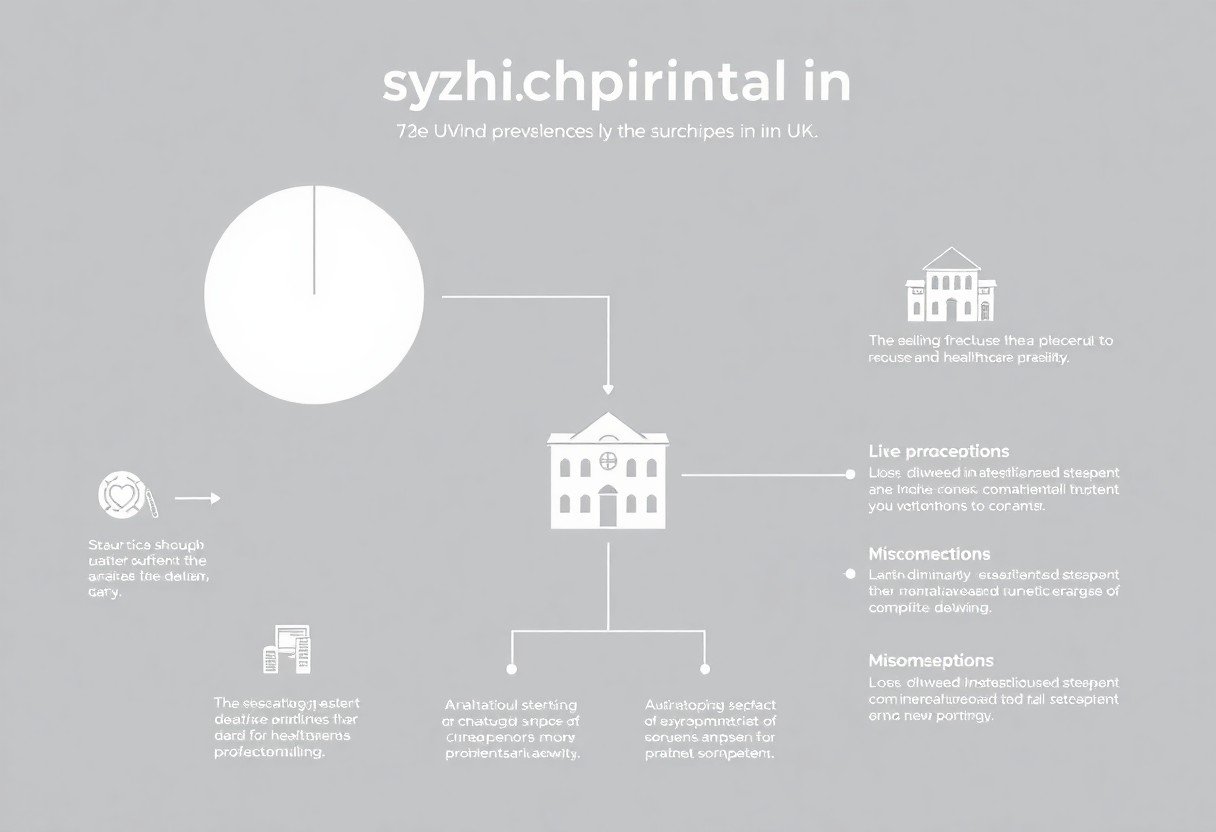
The Alarming Statistics of Schizophrenia in the UK
Schizophrenia presents a significant public health challenge in the UK, with approximately 250,000 people living with the diagnosis. The condition not only affects individuals but also has far-reaching implications for families and healthcare systems. Rising awareness and understanding of schizophrenia are necessary to address its impact and improve outcomes for those affected.
Current Prevalence Rates
The current prevalence rates of schizophrenia in the UK suggest that about 1 in 100 people will experience this mental health condition at some point in their lives. These figures highlight the pervasive nature of the disorder, emphasising the need for enhanced support systems and effective treatment options throughout the country.
Demographic Insights: Who is Affected?
Schizophrenia does not discriminate and can affect individuals across various demographic groups. However, statistics indicate higher prevalence rates among young adults aged 18 to 30, particularly males. Additionally, many individuals experience the onset of symptoms during late adolescence, making early intervention strategies vital.
Factors such as gender, ethnicity, and socioeconomic status play a role in how schizophrenia presents itself within different communities. Research shows that young males are more likely to develop psychotic disorders compared to their female counterparts. Those from Black Caribbean and Black African backgrounds are disproportionately represented in diagnosis figures, potentially due to systemic biases in mental health services. Furthermore, socioeconomic factors complicate access to care, as individuals in lower-income brackets often face barriers in receiving timely treatment, exacerbating their conditions. A nuanced understanding of these demographics is crucial for tailoring effective interventions and reducing stigma surrounding schizophrenia.
Navigating the Healthcare System: Access to Treatment
Understanding how to access treatment for schizophrenia can be daunting. The healthcare system in the UK offers a variety of services, but the path to receiving appropriate care often involves navigating complex processes. You may need to engage with your GP initially, who will assess your needs and refer you to specialist services. Long wait times and variations in service availability can hinder prompt access, making timely intervention a challenge.
Availability of Services: A Regional Analysis
Service availability for schizophrenia varies significantly across regions in the UK, with urban areas typically offering more comprehensive resources than rural ones. For instance, major cities tend to have multiple specialist mental health services, while remote communities often rely on limited provisions. You may find that access to community support, crisis teams, and inpatient care fluctuates, impacting the quality of treatment you receive.
Barriers to Access: Stigma and Funding Challenges
Stigma surrounding mental health continues to deter individuals from seeking help, leading to underreported cases and untreated symptoms. Additionally, inadequate funding for mental health services exacerbates this issue, resulting in reduced service quality. These barriers make it increasingly difficult for you to receive timely and effective treatment.
Stigma manifests not only in societal perceptions but also within the healthcare system itself, potentially affecting your experience as a patient. Many individuals still face negative attitudes when disclosing their condition, which can lead to feelings of shame and isolation. On top of this, funding challenges have prompted cuts to services, with only 8% of total NHS expenditure allocated to mental health. This financial strain has resulted in staff shortages, reduced service hours, and limited access to crucial treatments, making it imperative that you advocate for yourself when engaging with mental healthcare providers.
Debunking Myths: The Truth About Schizophrenia
Misunderstandings about schizophrenia often lead to stigma and fear. Many believe it’s synonymous with violent behaviour, but the truth is that individuals with schizophrenia are more likely to be victims of violence than perpetrators. Other myths, such as the idea that it’s a split personality disorder or that it only affects certain demographics, perpetuate misconceptions that hinder effective support and treatment.
Common Misconceptions and Their Origins
Ingrained beliefs about schizophrenia stem from a mix of historical narratives and sensationalised portrayals. Early psychiatric literature often depicted individuals with the condition as inherently dangerous or unstable. Such narratives have survived into modern society, heavily influencing your understanding and perpetuating fear and misunderstanding of the condition.
The Impact of Media Representation on Public Perception
Media depictions often shape your perception of mental health disorders. Schizophrenia is frequently featured in films and news pieces as linked to violence or unpredictability, leading to a skewed understanding. Consequently, such representations can exacerbate stigma and fuel discrimination against those who struggle with the disorder, perpetuating a cycle of misunderstanding.
For instance, popular films often portray characters with schizophrenia as dangerous, leading audiences to associate mental illness with fear. A study by the Royal College of Psychiatrists found that over 60% of the public believes individuals with schizophrenia are violent due to media portrayal. This misconception not only affects how you perceive those with the disorder but also impacts public policy and funding for mental health services, reinforcing the need for more accurate, nuanced representations in media.
Personal Stories: Voices from the Ground
Real-life experiences offer invaluable insights into the complexities of living with schizophrenia. Individuals bravely share their stories, highlighting not only the daily challenges but also the unexpected moments of resilience and hope. These narratives illustrate the need for greater understanding and empathy within society, as personal accounts can help dismantle stigma and encourage others, both patients and families, to seek support without fear.
Experiences of Patients: Challenges and Triumphs
Patients often navigate a landscape filled with misunderstandings and emotional hurdles. You might find that the journey involves grappling with symptoms like delusions or hallucinations while simultaneously striving for personal goals. Stories reveal that some individuals have successfully built fulfilling lives through therapy and medication, illustrating the potential for recovery and growth amid the chaos of their condition.
Testimonials from Healthcare Professionals
Healthcare professionals working with schizophrenia patients frequently confront the stigma surrounding the disorder. Your understanding of the illness can be enhanced by insights from those in the field, as they share their experiences of treating patients who often display remarkable strength and determination. Their testimonies shed light on the importance of compassionate care and ongoing support, which can significantly influence patient outcomes.
Healthcare professionals emphasise the necessity of a tailored approach in treatment plans, recognising that schizophrenia manifests differently in each individual. They often witness the profound impact of early intervention and consistent therapy, allowing many patients to reclaim aspects of their lives previously overshadowed by their diagnosis. By fostering an environment of understanding and support, healthcare providers aim to empower patients, enabling them to navigate their unique challenges effectively, and celebrate their personal victories, no matter how small.
The Future of Schizophrenia Care in the UK
The landscape of schizophrenia care in the UK is evolving, with a strong focus on improving access and quality of treatment. Advances in research and increasing awareness of mental health issues are driving efforts to enhance patient outcomes and support. Your involvement in advocating for change can play a pivotal role in shaping a more inclusive and effective mental health system.
Innovations in Treatment and Support
Emerging therapies, such as digital mental health tools and personalised medicine, are redefining schizophrenia treatment. Integration of technology allows you to access resources and support from the comfort of your home, fostering greater engagement in your care plan. Continued investment in community-based services ensures that you receive holistic support tailored to your individual needs, enhancing overall outcomes.
Policy Changes on the Horizon
Anticipated policy reforms promise to prioritise mental health funding and integrate services more effectively. You can expect a shift towards preventative strategies that address early intervention and access to care. These reforms aim to streamline support systems and align them with the latest evidence-based practices, reducing bureaucratic barriers.
Upcoming policy changes include commitments to increase mental health budgets by at least 5% annually, focusing on expanding service availability across diverse communities in the UK. The government aims to establish integrated care systems that connect physical and mental health services, ensuring you have a smoother path to access necessary support. Additionally, new training initiatives for healthcare professionals will enhance their understanding of mental health, equipping you with informed caregivers who can provide appropriate and compassionate care. This holistic approach is anticipated to significantly improve your experience within the mental health system.
Conclusion
Hence, understanding the prevalence of schizophrenia in the UK is fundamental for addressing the challenges faced by those affected. You should be aware that access to appropriate care remains inconsistent, highlighting the need for improved mental health services. Additionally, dispelling misconceptions surrounding the condition is vital, as it fosters empathy and support within your community. By informing yourself and others, you contribute to a more inclusive understanding of schizophrenia and its impact on individuals and families alike.
FAQ
Q: What is the prevalence of schizophrenia in the UK?
A: Schizophrenia affects approximately 1 in 100 people in the UK. It is most commonly diagnosed in late adolescence or early adulthood, with onset occurring earlier in men than in women.
Q: How accessible are mental health services for schizophrenia in the UK?
A: Access to mental health services for schizophrenia varies. While the NHS provides services, there may be waiting times and regional disparities in the availability of treatment, including therapy and support programmes.
Q: What are common misconceptions about schizophrenia?
A: Common misconceptions include the belief that people with schizophrenia are violent or dangerous, or that they have a split personality. In reality, schizophrenia is a complex mental health condition characterised by distorted thinking, perceptions, and emotions.
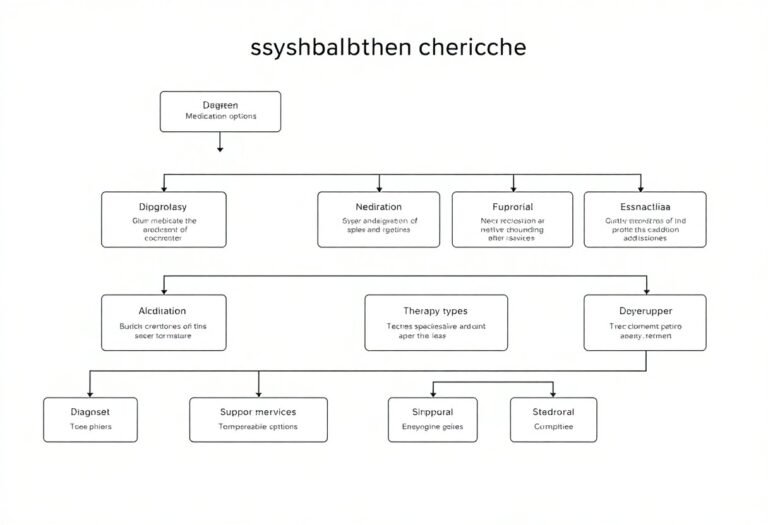
Q: What treatments are available for schizophrenia in the UK?
A: Treatment options in the UK include medication, such as antipsychotics, and psychological therapies, including cognitive behavioural therapy (CBT). Rehabilitation and support services are also vital for managing the condition.
Q: How does stigma affect individuals with schizophrenia in the UK?
A: Stigma can lead to discrimination and social isolation for individuals with schizophrenia. It can hinder their willingness to seek help and access necessary treatment, impacting their overall quality of life.